Qu’est-ce que la densité mammaire ?
La composition du sein est unique à chaque femme. Tous les seins contiennent des tissus graisseux, glandulaire et fibreux, mais les proportions varient d’une femme à l’autre et ne peuvent être déterminées qu’à l’aide d’une mammographie. On distingue quatre catégories de densité mammaire.
La composition des seins est unique à chaque femme. Tous les seins contiennent des tissus graisseux, glandulaire et fibreux, mais les proportions varient d’une femme à l’autre.
Les seins qui présentent une proportion plus élevée de tissu glandulaire et fibreux sont appelés seins denses.
Les seins denses sont fréquents. Chez les femmes âgées de 40 à 74 ans, 43 % ont des seins denses. En général, les seins deviennent moins denses et contiennent plus de tissu graisseux avec l’âge :
- 56% des femmes dans la quarantaine ont des seins denses.
- 37% des femmes dans la cinquantaine.
- 27% des femmes dans la soixantaine.
Avoir du tissu dense dans les seins est normal. Cependant, comprendre votre densité mammaire vous permet de mieux appréhender votre profil de risque et les implications, et de pouvoir prendre des décisions éclairées concernant le dépistage.
La densité mammaire ne peut être évaluée qu’à l’aide d’une mammographie. Un radiologue examine visuellement la répartition de vos tissus denses et graisseux (densité mammaire). Dans certaines provinces, un logiciel automatisé peut également effectuer ce calcul. La densité mammaire n’est pas corrélée à la taille ou à la fermeté des seins. Après un examen médical, certains professionnels de la santé peuvent informer une femme qu’elle a des seins denses. Toutefois, la densité mammaire ne peut être détectée par l’apparence ou la palpation.
Les seins denses ne doivent pas être confondus avec les seins bosselés.
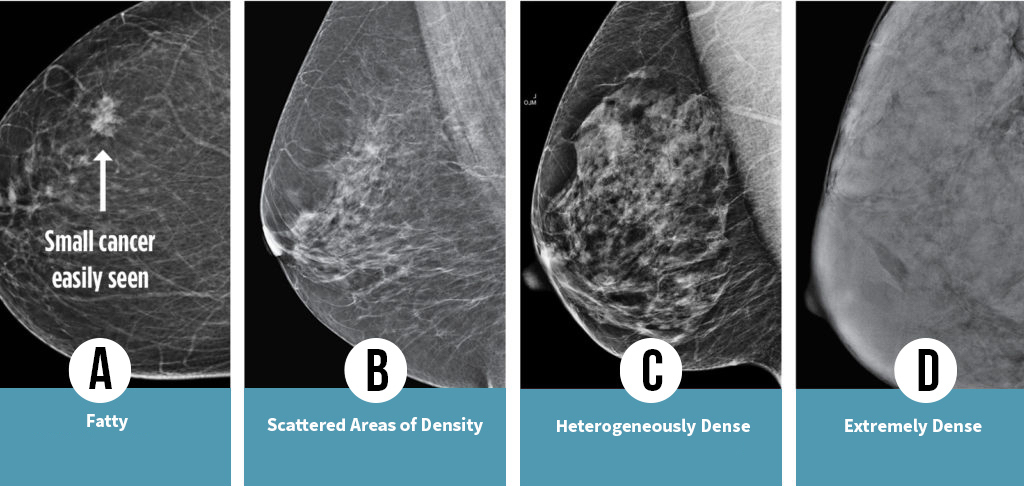 La densité mammaire varie selon le rang de la lettre. Elle est classée en quatre catégories : A, B, C et D. Certaines provinces distinguent aussi les catégories en utilisant des mots.
La densité mammaire varie selon le rang de la lettre. Elle est classée en quatre catégories : A, B, C et D. Certaines provinces distinguent aussi les catégories en utilisant des mots.
ON CONSIDÈRE QUE LES SEINS CLASSÉS EN CATÉGORIES C ET D PRÉSENTENT UNE DENSITÉ MAMMAIRE ÉLEVÉE.
Un tissu mammaire dense peut masquer de petites tumeurs, rendant la mammographie moins précise.
Catégorie A | seins presque entièrement graisseux
Les seins ont peu de tissus fibreux et glandulaires. Ils sont principalement composés de tissu graisseux. Une mammographie permettrait vraisemblablement de diagnostiquer une anomalie.
Catégorie B | seins composés de zones
de densités fibroglandulaires éparses
Les seins présentent des zones dispersées de tissus fibreux et glandulaire, ainsi qu’une bonne quantité de tissu graisseux.
Catégorie C | seins denses de façon hétérogène
Les seins ont une distribution régulière de tissus fibreux et glandulaires, ce qui rend difficile la détection de petites masses par mammographie.
Catégorie D | seins extrêmement denses
Les seins sont composés de tissus fibreux et glandulaires abondants, ce qui rend encore plus complexe la détection d’une tumeur maligne par mammographie.
À quel groupe appartenez-vous ? Une mammographie de dépistage sera nécessaire pour le déterminer.
Les chiffres ci-dessous peuvent fluctuer en fonction de la province et du recours à un programme informatique pour mesurer la densité lors d’une mammographie, ou encore en raison de l’évaluation subjective effectuée par le radiologue.
- 10 % se situent dans la catégorie de densité la plus faible, caractérisée par une prédominance de tissu graisseux.
- 40% se situent dans la catégorie de seins composés de zones de densités fibroglandulaires éparses.
- 40% se situent dans la catégorie de seins denses de façon hétérogène (catégorie C, considérée comme seins denses).
- 10% se situent dans la catégorie de seinsextrêmement denses (catégorie D) (seins considérés comme denses).
Plus votre densité mammaire est élevée, plus le risque qu’une tumeur passe inaperçue est grand et plus le risque de cancer du sein est accru.
ÂGE : Les seins denses sont plus courants chez les jeunes femmes. Cependant, en vieillissant, la densité mammaire ne diminue pas nécessairement.
- 56 % des femmes de la quarantaine ont les seins denses.
- 37 % des femmes de la cinquantaine.
- 27 % des femmes de la soixantaine.
MÉNOPAUSE : Après la ménopause, la densité mammaire peut diminuer mais ce n’est pas toujours le cas.
ETHNICITÉ : Chez les femmes d’origine asiatique ont retrouve un pourcentage élevé de seins denses.
HÉRÉDITÉ : La densité mammaire peut être transmise génétiquement.
HTS : Accroissement de la densité chez les femmes recevant une hormonothérapie de remplacement.
TAILLE DES SEINS : Une poitrine plus petite est corrélée à une densité mammaire plus élevée.
GROSSESSE ET ALLAITEMENT : Pendant cette période, les seins gagnent en densité.
POIDS : Une masse corporelle élevée est inversement corrélée à la densité.
INHIBITEURS DE L’AROMATASE ET TAMOXIFÈNE : Ces médicaments utilisés pour traiter le cancer font diminuer la densité.
Selon certaines recherches, les mammographies conventionnelles peuvent diminuer le taux de mortalité lié au cancer du sein, même chez les femmes qui n’ont pas des seins très denses. Cependant, il est crucial de souligner que la densité mammaire n’est pas le seul facteur de risque. D’autres facteurs peuvent également contribuer à l’apparition d’un cancer du sein, même chez les femmes dont la densité mammaire est faible. N’hésitez pas à en parler avec votre médecin ou votre infirmière praticienne.
Veuillez remplir l’évaluation du risque de cancer du sein IBIS, qui peut être effectuée de manière autonome ou avec l’aide d’un professionnel de la santé. Les femmes présentant un risque accru de cancer du sein tireront souvent profit d’une imagerie par résonance magnétique (IRM) en plus d’une mammographie. En Ontario et en Nouvelle-Écosse, on considère qu’un risque élevé de développer un cancer du sein au cours de sa vie existe lorsque ce risque dépasse 25 %. En Alberta et aux États-Unis, le seuil est fixé à 20 %. Quel est le risque que vous soyez atteinte d’un cancer du sein au cours de votre vie ? Découvrez l’outil d’évaluation du risque de cancer du sein IBIS : https://magview.com/ibis-risk-calculator/

Pourquoi est-il important de connaitre ma densité mammaire ?
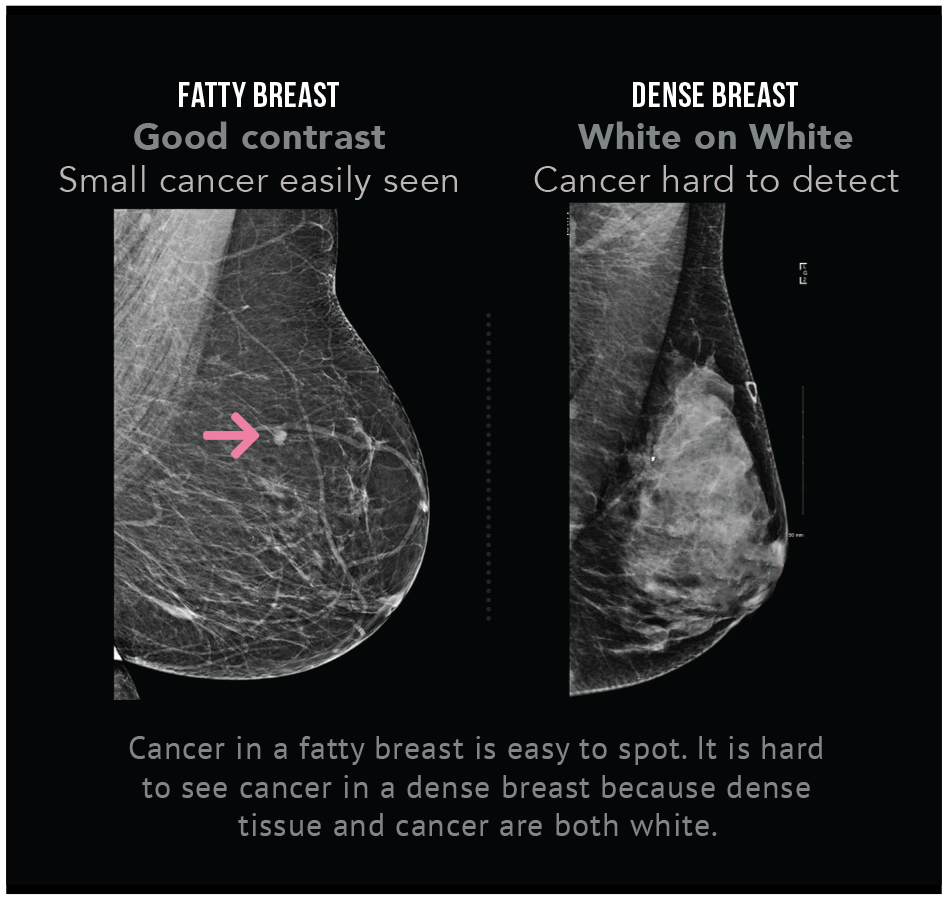
La détection du cancer par les médecins est rendue plus difficile en présence de seins denses, car un effet de camouflage fait que la tumeur et le tissu mammaire dense apparaissent tous deux en blanc sur une mammographie.
La densité mammaire élevée complique la détection du cancer du sein, car la tumeur et le tissu dense ont tendance à apparaître tous deux en blanc sur une mammographie, ce qui crée un effet de camouflage. À l’inverse, dans un sein principalement composé de tissus graisseux, le tissu graisseux laisse mieux passer les rayons X et se présente en noir ou en gris, ce qui améliore le contraste et facilite l’identification des anomalies. 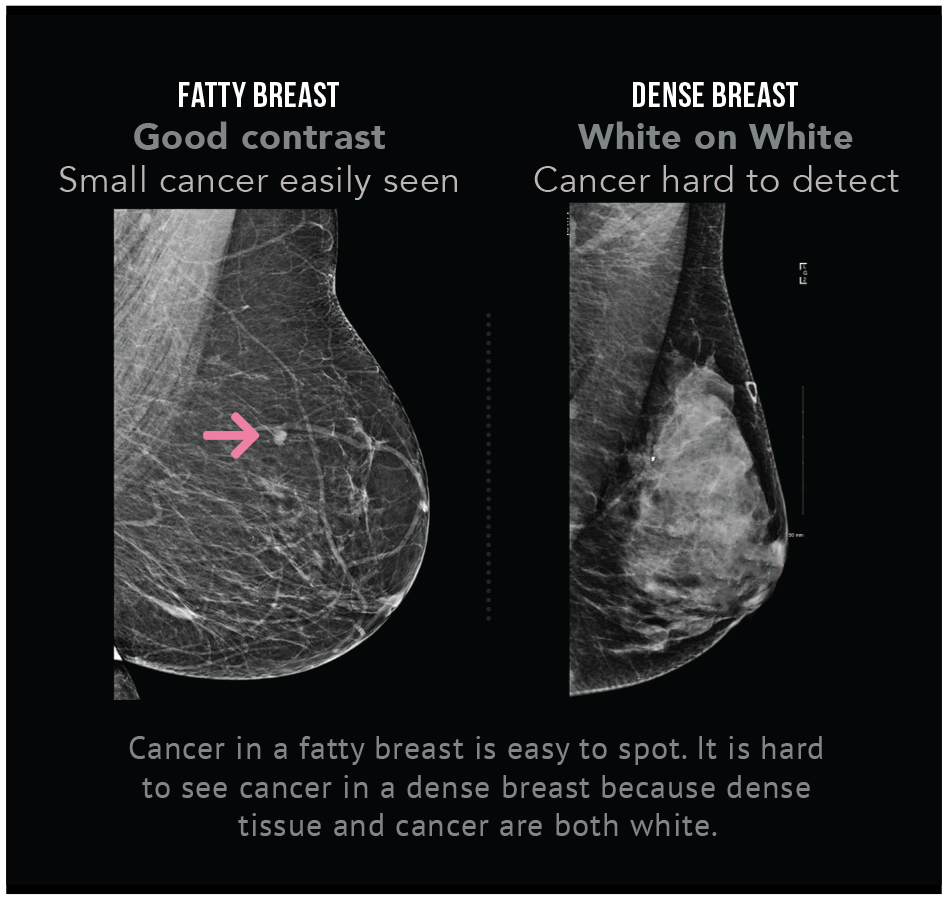
Dans le dépistage du cancer du sein, la tomosynthèse (mammographie 3D) est-elle plus efficace que la mammographie conventionnelle pour détecter un cancer dans un sein dense ?
La tomosynthèse, une forme avancée de mammographie en trois dimensions, est actuellement utilisée comme outil de dépistage dans certaines provinces. Toutefois, sa principale utilisation réside dans le diagnostic. Bien qu’elle puisse identifier un ou deux cancers invasifs supplémentaires chez mille femmes, il est important de noter que son efficacité diminue proportionnellement à la densité mammaire. En effet, cette technique de détection montre une capacité réduite à repérer des tumeurs chez les femmes présentant des seins très denses (catégorie D).
En effet, l’échographie additionnelle détecte plus de tumeurs cancéreuses que la tomosynthèse. Selon les informations recueillies au cours des 40 dernières années, la mammographie s’avère insuffisante pour les femmes présentant une densité mammaire élevée.
Les deux principaux facteurs de risque de développer un cancer du sein sont le fait d’être une femme et le vieillissement. Le risque augmente aussi en cas de densité mammaire élevée.
Une récente étude de grande envergure a révélé que la densité mammaire est un facteur de risque plus courant que les antécédents familiaux. Plus la densité est élevée, plus le risque de développer un cancer du sein augmente.
Les femmes ayant une densité mammaire élevée (catégorie D) présentent un risque de cancer du sein quatre à six fois plus élevé que celles dont la densité est la plus faible (catégorie A).
Malheureusement, les mammographies ne détectent pas environ 40 % des cancers chez les femmes à forte densité mammaire, ce qui entraîne souvent un diagnostic tardif et peut compromettre les chances de guérison.
Références :
Boyd, N., Guo, H., Martin, L., Sun, L., Stone, J., Fishel, E., Jong, R., Hislop, G., Chiarelli, A., Minkin, S., et Yaffe, M. (janvier 2007). Mammographic density and the risk and detection of breast cancer. New England Journal of Medicine, 356:227-236. Consulter l’étude Voir l’étude
Engmann N., Golmakani M., Miglioretti D., Sprague B., Kerlikowske K., pour le Breast Cancer Surveillance Consortium. (2 février 2017). Population-Attributable Risk Proportion of Clinical Risk Factors for Breast Cancer. JAMA Oncol Consulter l’étude Voir l’étude
Découvrir ma densité
How can I find out my density?
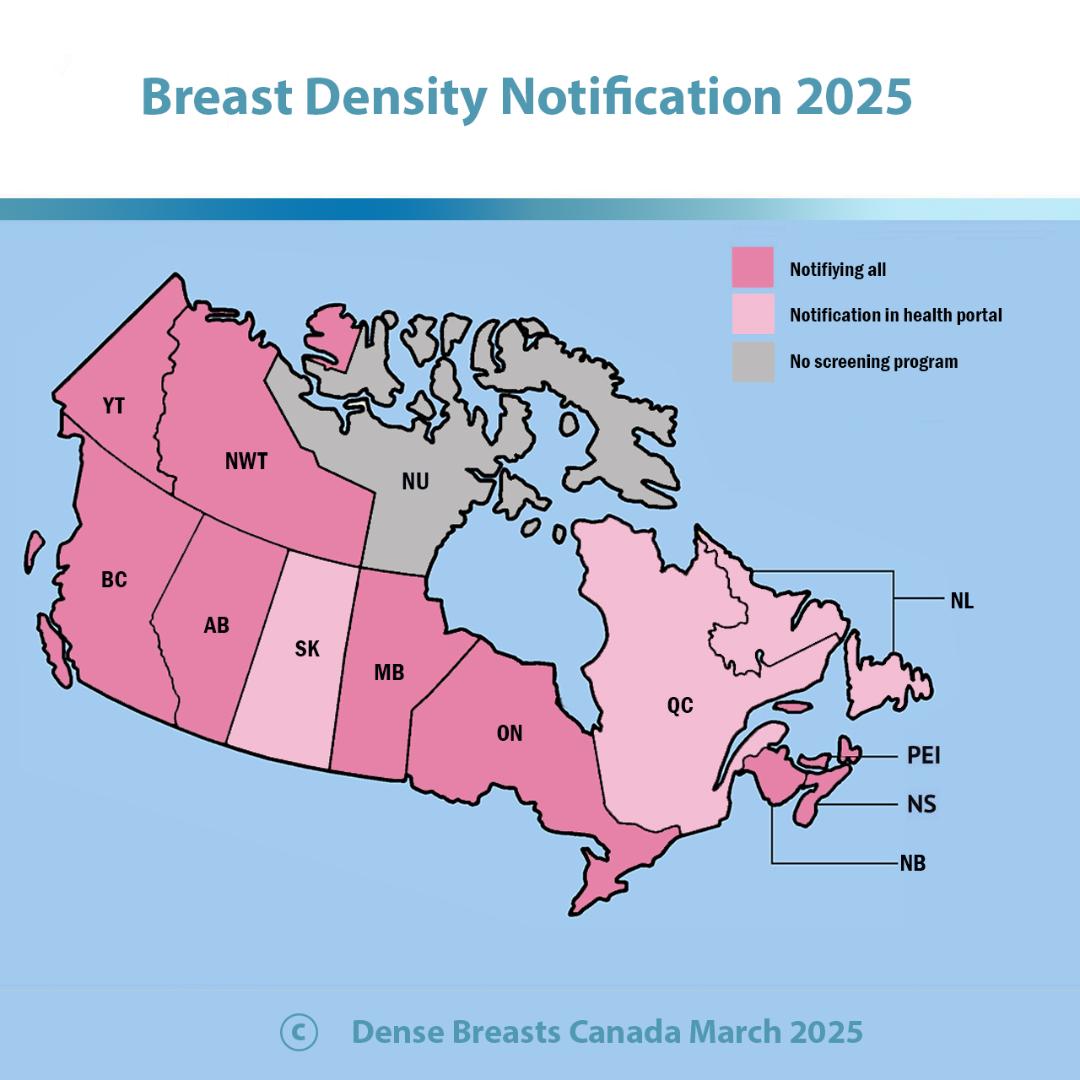
Dense Breasts Canada was successful in getting breast density notification implemented on Oct.1, 2020. Anyone having a screening mammogram will be informed of their breast density category in their mammogram results letter: A, B, C, or D. Check your letter that comes in the mail.
Category C and D are dense breasts and women in these categories can benefit from additional screening.
Your healthcare provider also receives a report that has your density category.
What should I do if I have dense breasts?
1. Please discuss optimal screening for you with your provider, based on all your risk factors. Having dense breasts increases your risk, but you may have other risk factors to consider.
2.The IBIS risk calculator is recommended and can be found https://magview.com/ibis-risk-calculator/ When doing the risk calculator, anyone with a lifetime risk of over 20% is considered high risk. MRI is used. When using the calculator, click the word BIRADS. Category C is called heterogeneously dense and Category D is called extremely dense. (note: Alberta is the only province that considers over 20% lifetime risk for MRI).
3. Consider additional screening: The Alberta Screening Program recommendation for healthcare providers states: For women with Category D: annual mammography and consider annual breast ultrasound and annual clinical exam. Note: Experts recommend screening ultrasound or MRI for women with both Category C and D dense breasts.
Currently, these clinics have let us know that they offer screening ultrasound to women with dense breasts, paid for by Alberta Health Services:
Mayfair, Canada Diagnostics, EFW, Pureform Radiology, Central Alberta Medical Imaging Services, Beam Radiology, Calgary Women's Imaging Clinic, Insight Medical Imaging, and MIC Medical Imaging. It is your choice where to get screened.
4. Practice self-exam and consider modification of lifestyle factors.
Plaidez en faveur d'un changement en Alberta en leur envoyant cette lettre.
Breast density notification was implemented only for women with Category D density in Nov. 2018. As of December 2022, anyone can learn their breast density category in one of two ways:
1. You can ask your healthcare provider; they are now told your density category or
2. Allez dans votre MySaskHealthRecord et consultez votre catégorie de densité sur le rapport de mammographie.
Upcoming changes: The Saskatchewan screening program is updating its system to be able to notify all individuals having a screening mammogram of their breast density in the results letter mailed to them after a screening mammogram. The update will be completed in June 2025.
Additional Screening: Individuals with Category D are asked to return annually for a mammogram.
If you have Category C or D density, you have dense breasts. Please also consider requesting supplemental screening, ie. ultrasound or MRI.
Please discuss optimal screening for you with your provider, based on all your risk factors.
What is your risk?
Having dense breasts increases your risk, but you may have other risk factors to consider. The IBIS risk calculator is recommended and can be found https://magview.com/ibis-risk-calculator/ When doing the risk calculator, anyone with a lifetime risk of over 25% is considered high risk. MRI is used. Please click the words BIRADS when you see it and note that Category C is called heterogeneously dense and Category D is called extremely dense.
Screening at 40: Begins Jan 2025. You will be able to self-refer for a mammogram starting at age 40.
Plaider pour le changement au Saskatchewan en envoyant une lettre à votre Ministre de la Santé. lettre..
Dense Breasts Canada and patient advocates were successful in getting breast density notification implemented on Jan. 5, 2021. Anyone having a screening mammogram will be informed of their breast density category in the mammogram results letter mailed to them: A, B, C or D. Category C and D are dense breasts.
Evidence shows ultrasound or MRI are recommended for women with dense breasts as they find additional cancers that have been missed on mammogram.
Please discuss optimal screening for you with your provider, based on all your risk factors.
What is your risk?
Having dense breasts increases your risk, but you may have other risk factors to consider. The IBIS risk calculator is recommended and can be found https://magview.com/ibis-risk-calculator/ When doing the risk calculator, anyone with a lifetime risk of over 25% is considered high risk. Please click the words BIRADS when you see it and note that Category C is called heterogeneously dense and Category D is called extremely dense.
Plaider pour le changement au Manitoba en les envoyant cette lettre..
Update: Dense Breasts Canada's advocacy has been successful in Ontario. All women having a screening mammogram are directly informed of their breast density in their mammogram results letter mailed to them. This began July 21, 2023. If you had a mammogram before this date, you can find out your breast density category by asking your health care provider: is it A, B, C, or D?
Category C and D are dense breasts and women with dense breasts can benefit from additional screening.
If you do not have a healthcare provider, you can call the OBSP and they will tell you your density: 1 800 668 9304
Currently, only women with Category D are asked to return annually for a mammogram, instead of every two years. However, dense breasts refer to Category C as well. Women with Category C should consider requesting additional screening, such as ultrasound or MRI. If your healthcare provider will not provide you with a requisition for additional screening, please take a look at our conversation tips in the footer of the website. There is also a clinic in downtown Toronto that offers Automated Breast Ultrasound privately.
NEWS: In December 2023 Ontario Health announced a recommendation for additional screening for individuals with Category D. The recommendation is now being implemented. You can request a MRI every 2 years or a mammogram with ultrasound every year. You need a requisition from your healthcare provider. Read more here and you can print this off for your provider too. https://www.cancercareontario.ca/en/guidelines-advice/cancer-continuum/screening/breast-density-provider-information
Please discuss optimal screening for you with your provider, based on all your risk factors.
What is your risk?
Having dense breasts increases your risk, but you may have other risk factors to consider. The IBIS risk calculator is recommended and can be found https://magview.com/ibis-risk-calculator/ When doing the risk calculator, anyone with a lifetime risk of over 25% is considered high risk. Please click the words BIRADS when you see it and note that Category C is called heterogeneously dense and Category D is called extremely dense.
Lisez notre communiqué de presse sur la notification de la densité mammaire:
Communiqué de presse sur la notification de la densité mammaire en Ontario 24 juillet 2023.
QUÉBEC: Your mammogram report sent to your healthcare provider has a description of your density in percentages. Every report has the density. You will NOT be notified directly but you can find out your density by asking. The density information is on the third line of the report. Women with over 75% density and a family history are offered screening ultrasound.
Please discuss optimal screening for you with your provider, based on all your risk factors.
What is your risk?
Having dense breasts increases your risk, but you may have other risk factors to consider. The IBIS risk calculator is recommended and can be found https://magview.com/ibis-risk-calculator/ When doing the risk calculator, anyone with a lifetime risk of over 25% is considered high risk. Please click the words BIRADS when you see it and note that Category C is called heterogeneously dense and Category D is called extremely dense.
We continue to advocate for direct notification and if you would like to express your concerns about the withholding of health information, please contact The Health Minister, The Honourable Christian Dubé
ministre@msss.gouv.qc.ca
Plaidez pour un changement au Québec en leur envoyant cette lettre..
NOUVELLE-ÉCOSSE: Dense Breasts Canada was successful in getting breast density notification implemented in Nova Scotia October 29, 2019. Anyone having a screening mammogram will be informed of their breast density category in their mammogram results letter: A, B, C, or D. Category C and D are dense breasts.
As of 2023, individuals with Category D density are offered annual mammograms.
Please discuss optimal screening for you with your provider, based on all your risk factors.
What is your risk?
Having dense breasts increases your risk, but you may have other risk factors to consider. The IBIS risk calculator is recommended and can be found https://magview.com/ibis-risk-calculator/ When doing the risk calculator, anyone with a lifetime risk of over 25% is considered high risk. Please click the words BIRADS when you see it and note that Category C is called heterogeneously dense and Category D is called extremely dense.
Please note: Women with dense breasts can benefit from additional screening, such as ultrasound. However, GP requisitions for ultrasound are refused. This is the only province where this is happening. If you would like to help us advocate, please contact us at info@densebreastscanada.ca and please contact Premier Tim Houston premier@novascotia.ca to tell him that this situation is putting women's lives at risk. We also have a letter in the footer of our website.
July 2024 Letter to Premier Houston:
Powerpoint Presentation to Nova Scotia MLAs on the need for additional screening. https://www.densebreastscanada.ca/wp-content/uploads/2024/02/Nova-Scotia-Presentation-The-need-for-additional-screening-for-women-with-dense-breasts-Feb-23-2024.pptx
Briefing Note: https://www.densebreastscanada.ca/wp-content/uploads/2024/03/Nova-Scotia-Breast-Cancer-Screening-Issues-2024.docx
Communiqué de presse sur la notification de la densité mammaire
NOUVEAU-BRUNSWICK: Breast density notification for all women was implemented in New Brunswick in July 2020. You will be informed of your breast density category in your mammogram results letter: A, B, C, or D. Category C and D are dense breasts.
Please discuss optimal screening for you with your provider, based on all your risk factors. Women with dense breasts can benefit from additional screening, i.e. ultrasound or MRI.
There is difficulty accessing ultrasound and MRI in New Brunswick. There is a private option for MRI but not ultrasound in Moncton. The cost is $900. You can contact IRM MONCTON MRI 585, Mapleton Rd. suite 101 Moncton, NB
www.irmmonctonmri.com We are not affiliated.
What is your risk?
Having dense breasts increases your risk, but you may have other risk factors to consider. The IBIS risk calculator is recommended and can be found https://magview.com/ibis-risk-calculator/ When doing the risk calculator, anyone with a lifetime risk of over 25% is considered high risk. MRI is used for this category. Please click the words BIRADS when you see it and note that Category C is called heterogeneously dense and Category D is called extremely dense.
New Brunswick Breast Density Notification Press Release
PEI: Breast density notification for all women was implemented in January 2020. You will be informed of your breast density category in your mammogram results letter: A, B, C or D. Category C and D are dense breasts. Women with dense breasts can benefit from additional screening.
The government committed to screening ultrasound for women in Category D in 2018 and has not kept its commitment.
Please discuss optimal screening for you with your provider, based on all your risk factors.
What is your risk?
Having dense breasts increases your risk, but you may have other risk factors to consider. The IBIS risk calculator is recommended and can be found https://magview.com/ibis-risk-calculator/ When doing the risk calculator, anyone with a lifetime risk of over 25% is considered high risk and MRI is used. Please click the words BIRADS when you see it and note that Category C is called heterogeneously dense and Category D is called extremely dense.
TERRE-NEUVE-ET-LABRADOR
You are not provided with any information at this time, but change is underway. Currently, your healthcare provider is notified of your density category: A, B, C or D. Women in Category D are notified in the mail and asked to return for an annual mammogram.
A software update is under way and it is expected that all women will be informed of their breast density category in their mammogram results letter: A, B, C or D as of Fall 2024.
Please check with your GP for your breast density in the interim and discuss optimal screening for you, based on all your risk factors. Women with dense breasts can benefit from additional screening.
What is your risk?
Having dense breasts increases your risk, but you may have other risk factors to consider. The IBIS risk calculator is recommended and can be found https://magview.com/ibis-risk-calculator/ When doing the risk calculator, anyone with a lifetime risk of over 25% is considered high risk. MRI is used. Please click the words BIRADS when you see it and note that Category C is called heterogeneously dense and Category D is called extremely dense.
How can I find out my density?
Dense Breasts Canada was successful in getting breast density notification implemented on Oct.15, 2018. Anyone having a screening mammogram will be informed of their breast density category: A, B, C, or D in their results letter. Check the letter that comes in the mail.
Category C and D are dense breasts and women in these categories can benefit from additional screening.
Your healthcare provider also receives a report that has your density category.
What should I do if I have dense breasts?
1. Please discuss the screening that best meets your needs with your provider, based on ALL your risk factors. Having dense breasts increases your risk, but you may have other risk factors to consider as well.
2.The IBIS risk calculator is recommended and can be found https://magview.com/ibis-risk-calculator/ When doing the risk calculator, anyone with a lifetime risk of over 25% is considered high risk. MRI is used. When using the calculator, click the word BIRADS. Category C is called "Heterogeneously dense" and Category D is called "Extremely dense."
3. Practice self-exam as mammogram accuracy is less in dense breasts. Consider modification of lifestyle factors.
4. Consider additional screening. Experts recommend ultrasound or MRI (depends on overall risk) for women with both Category C and D dense breasts. You can request a requisition from your healthcare provider.
Currently, these locations offer screening ultrasound to women with dense breasts, paid for by MSP. A requisition is needed.
Vancouver: X-ray 505. Note screening ultrasound is only available for patients who have their mammograms there. Please book mammogram and then you will be able to have an ultrasound at the halfway mark of your screening protocol ( ultrasound at 1 year mark if you go for mammogram every 2 years and ultrasound at 6 month mark if you go for mammogram every year.
Victoria: 1. West Coast Medical Imaging, Fort St. -uses 3D Automated Breast Ultrasound
Victoria: 2. Victoria General Hospital for Victoria residents
Prince George: University Hospital of Northern British Columbia
Vernon: Vernon Jubilee: Category D only
Kamloops: Royal Inland Hospital: Category D. Also available for Category C patients with a lifetime risk of breast cancer calculated at >20-25%.
Nainaimo: Nanaimo Regional General Hospital: MRI for Category D
Shuswap Lake: Shuswap Lake General Hospital if mammogram is done at Vernon or Salmon Arm. Offers ultrasound for Category D.
Port Alberni: West Coast General Hospital.
Chilliwack: Chilliwack General Hospital: Ultrasound for Category C and D only for patients with a 1st degree relative with breast cancer or tested positive for BRCA gene
This list was last updated Dec 2025. Please let us know of any additional locations.
Please sign this letter to the government asking for increased access
Communiqué de presse sur la notification de la densité mammaire en Colombie-Britannique
Advocate for more access to additional screening in British Columbia in by sending them this letter.
Territoires du Nord-Ouest: As of March 1, 2024 All women having a screening mammogram are notified of their breast density in the mammogram results letter mailed to them. Category C and D are considered to be dense breasts. Women assessed as category D density are asked to return for annual mammograms. Women with dense breasts can benefit from supplemental screening ultrasound. This is available for women with Category D density and is an official guideline from the Dept of Health.
Yukon: As of January 1, 2024: All women having a screening mammogram are notified of their breast density in the mammogram results letter mailed to them. Category C and D are considered to be dense breasts. Women assessed as category D density are asked to return for annual mammograms. Women with dense breasts can benefit from supplemental screening ultrasound, however this is not available in the Yukon at this time.
Et si j’ai les seins denses?
Discutez de votre catégorie de densité et de tout autre facteur de risque comme la génétique, les antécédents familiaux et les biopsies précédentes afin de comprendre votre risque global de cancer.
Discutez de votre catégorie de densité et de tout autre facteur de risque comme la génétique, les antécédents familiaux et les biopsies précédentes afin de comprendre votre risque global de cancer.
Si vous avez des seins denses, parlez à votre médecin ou à votre infirmière praticienne au sujet d’examens de dépistage supplémentaires comme l’échographie puisqu’une mammographie NORMALE pourrait être fausse. Les tissus denses peuvent masquer le cancer. L’échographie permet de détecter des cancers supplémentaires. Vous êtes le meilleur plaidoyer pour votre santé et vous devriez peut-être demander des examens supplémentaires.
COMMENT PLAIDER EN FAVEUR D’UN DÉPISTAGE SUPPLÉMENTAIRE?
Si vous désirez subir un examen de dépistage supplémentaire, faites-vous entendre et faites savoir il est important de signaler à votre médecin ou à votre infirmière praticienne que vous connaissez les risques suivants:
- Il y a un risque de cancer plus élevé associé aux seins denses. Les seins denses sont en soi un facteur de risque. La densité mammaire est un facteur de risque nettement plus fréquent que l’histoire familiale.
- En présence de seins denses, les mammographies traditionnelles ne sont pas fiables à cause de leur effet de camouflage. Le cancer et le tissu mammaire paraissent tous les deux blancs lors d’une mammographie. Cela touche aux deux catégories de seins denses.
- Il y a chez les femmes avec les seins denses un niveau élevé de cancers d’intervalle – les cancers détectés entre les tests de dépistage lorsqu’une femme sent une masse suite à des résultats négatifs d’une mammographie.
- La capacité avérée des échographies et des IRM à détecter d’autres tumeurs cancéreuses non identifiées au préalable par une mammographie.
Rappelez-vous : dans la plupart des cas, lorsqu’un examen de dépistage supplémentaire est effectué, on NE DÉCOUVRE PAS de cancer du sein.
- Parlez avec votre médecin de votre densité mammaire, de tous les facteurs de risque liés au cancer du sein et de vos meilleures options de dépistage.
- Effectuez régulièrement un auto-examen entre les examens de dépistage. Un résultat de mammographie normal pourrait ne pas être exact.
- Pour améliorer le dépistage précoce, envisagez des examens supplémentaires, comme l’échographie ou une imagerie par résonance magnétique (IRM) si vous présentez un risque élevé.
- Envisagez des changements liés à votre style de vie comme l’alimentation, l’exercice, la consommation d’alcool et la thérapie hormonale pour diminuer votre risque de cancer.
- Continuez de passer des mammographies, car elles permettent de détecter les calcifications, qui peuvent être le signe le plus précoce de cancer.
L’échographie peut détecter un petit cancer à un stade précoce avant qu’il ne se propage dans les ganglions lymphatiques.
Les études montrent que pour chaque 1 000 femmes examinées et qui présentent des seins denses, ultrasound finds another 2-3 cancers qui n’étaient pas visibles sur une mammographie.
Plusieurs études à grande échelle révèlent qu’ une échographie en complément à une mammographie peut augmenter la détection de cancer jusqu’à 97 % chez les femmes avec des seins denses.
On sait depuis 1995, date à laquelle le premier article a été publié dans la revue Cancer que l'échographie est capable de détecter des cancers avec de petits ganglions invasifs négatifs chez les femmes avec des seins denses.
Au Japon, un dépistage par échographie supplémentaire est enclenché et il permet une meilleure détection des cancers et une réduction de leurs intervalles d'apparition.
L’échographie est utilisée lorsqu’une anomalie est détectée au moyen d’une mammographie ou d’un examen clinique. Elle n’est pas utilisée dans le cadre du dépistage, car il s’agit d’un examen qui peut être influencés par plusieurs facteurs, donnant ainsi lieu à de faux positifs c'est-à-dire. une anomalie autre que le cancer. Les faux positifs sont inévitables lors du dépistage et très peu de tests identifieront un cancer. Si vous voulez passer une échographie, faites-en la demande et défendez vos droits. Les échographies, en plus des mammographies, sont importantes pour les femmes avec des seins denses, car les mammographies peuvent ne pas détecter les cancers en raison de l’effet de camouflage des tissus denses.
Si vous avez des seins denses et souhaitez passer une échographie, mais que votre médecin/infirmière praticienne refuse de vous la prescrire, veuillez consulter nos conseils de conversation sur ce qu'il faut dire. Pour défendre efficacement votre cause, nous avons préparé cette liste d'arguments potentiels auxquels vous pourriez être confrontée. La science est de votre côté et des décennies de preuves démontrent les avantages de l'échographie. Voici la liste de conseils. https://densebreastscanada.ca/wp-content/uploads/2022/02/Script-for-women-with-dense-breasts-who-want-a-screening-ultrasound.pdf
If you like, you can look into private facilities in your province that offer ultrasound without a doctor’s requisition.
Résidents de l’Ontario: There is a private clinic in Toronto 3D Automated Breast Ultrasound (ABUS). Private insurance may cover some of the cost. ABUS was approved by Health Canada in 2011 as a screening tool. You do not need a doctor’s/nurse practitioner’s referral. More information about private options can be found in the Screening Options Section.
Résidents de la Colombie-Britannique: MISE À JOUR en janvier 2019. Si votre médecin ou infirmière praticienne vous recommande de passer une échographie, le régime des soins médicaux couvre désormais l’échographie de dépistage chez les femmes avec des seins denses. Si ce n'est pas le cas, il existe des centres d'imagerie qui offrent des échographies par système portatif sans recommandation. En Colombie-Britannique, si l’échographie de dépistage ne vous a pas été recommandée, vous devrez défrayer les coûts (environ 250 $).
Vous avez des seins denses et on vous refuse une échographie de dépistage ou vous souhaitez une échographie. Vous avez passé une mammographie et avez appris que vous aviez des seins denses. Comme les tissus denses peuvent masquer un cancer sur une mammographie, vous souhaitez bénéficier d'un dépistage supplémentaire. Vous avez besoin d'une demande d'échographie de dépistage, mais votre prestataire de soins de santé ne veut pas vous en fournir une ou doit être convaincu. Nous avons conçu un script pour vous aider à défendre vos intérêts et à surmonter les obstacles potentiels lors d'une conversation avec votre prestataire de soins de santé.
Si votre fournisseur de soins de santé vous dit : Les lignes directrices canadiennes sur le dépistage du cancer du sein ne recommandent pas les échographies de dépistage pour les femmes ayant des seins denses.
Vous pouvez répondre : Je comprends que c'est la recommandation, mais comme il y a un risque accru de cancer avec les seins denses et que les mammographies ne sont pas aussi efficaces à cause de l'effet de masque, j'aimerais programmer une échographie pour être sûre.
Informations complémentaires : Depuis 1995, de nombreuses études ont démontré que l'échographie permet de détecter d'autres tumeurs cancéreuses non détectées par la mammographie[1].
Si votre prestataire de soins de santé vous dit : "Vous n'avez pas d'antécédents familiaux ou d'autres facteurs de risque : Vous n'avez pas d'antécédents familiaux ni d'autres facteurs de risque et vous n'avez donc pas besoin de vous préoccuper d'un dépistage supplémentaire.
Vous pouvez répondre : Les seins denses sont en fait un facteur de risque plus répandu que les antécédents familiaux[2] La plupart des femmes chez qui l'on diagnostique un cancer du sein n'ont aucun facteur de risque dont elles soient conscientes. J'aimerais prendre rendez-vous pour une échographie.
**If it applies to you, you can remind your health care provider that Black, Asian and Hispanic women are at an increased risk for breast cancer at a younger age than white women.[3]
**Si vous êtes concernée, vous pouvez rappeler à votre médecin que les femmes noires, asiatiques et hispaniques sont plus exposées au risque de cancer du sein à un âge plus jeune que les femmes blanches[3].
Vous pouvez répondre : Je comprends qu'il est possible que d'autres tests soient nécessaires si quelque chose est détecté, mais je ne suis pas très inquiet à l'idée d'être rappelé. Je préfère prévenir que guérir. Je comprends que toute anxiété que j'éprouverai sera de courte durée si j'obtiens un résultat normal. Et si le résultat n'est pas normal, je préfère que le cancer soit détecté à un stade précoce plutôt qu'à un stade plus avancé. J'aimerais donc prendre rendez-vous pour une échographie.
[1] https://acsjournals.onlinelibrary.wiley.com/doi/abs/10.1002/1097-0142(19950815)76:4%3C626::AID-CNCR2820760413%3E3.0.CO;2-Z
[2] https://jamanetwork.com/journals/jamaoncology/article-abstract/2599991
[3] https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5875337/?tool=pmcentrez&report=abstract
L’échographie 3D, également connue sous le nom d’échographie automatisée des seins (ABUS), utilise des ondes sonores. Des milliers d’images sont créées et un logiciel les reconstruit pour faire une image en 3D.
Automated Breast Ultrasound (ABUS) a été approuvée par Santé Canada comme outil de dépistage en 2011 et comme complément à la mammographie pour les femmes ne présentant aucun symptôme de cancer du sein. Les preuves montrent qu'il détecte jusqu'à 3,6 cancers supplémentaires pour 1000 femmes dépistées. Il est actuellement disponible dans les cliniques privées à Toronto. Il est facilement disponible en Alberta et payé en vertu de l'assurance provinciale.
Une assurance privée peut couvrir une partie des coûts en Ontario. Vous n'avez pas besoin de recommandation d'un médecin ou d'une infirmière praticienne si vous payez en privé en Ontario.
OUI! Les mammographies réduisent le nombre de décès attribuables au cancer du sein. Les mammographies peuvent détecter en toute fiabilité les calcifications suspectes. L’échographie et l’ABUS ne remplacent pas la mammographie; on les utilise en complément à la mammographie.
A breast cancer risk calculator is a tool that can help you and your doctor better understand your risk and make informed decisions. We’re posting the TYRER-CUZICK 8 model because it’s just been updated to include breast density as a risk factor. You can do the calculator on your own and message us if you have any questions.
If you don’t know your density, you can still use it and retry it when you find out your density. The model calculates 10 year risk and lifetime risk. In AB, lifetime risk over 20% is considered high risk and in ON and NS , 25% lifetime risk is considered high risk and there is a specialized high risk program in NS and ON. Elsewhere: If your lifetime risk is over 20 or 25% please speak to your provider about policies in your province Check out calculator here.
Women who have breast cancer are at higher risk of getting a second cancer in the same breast or the opposite breast. Women who have breast cancer and have dense tissue are at higher risk of getting breast cancer in the other breast than a woman with non-dense breasts. Patients with high density have a much greater risk of local recurrence compared with women with the least dense breasts (21% compared with 5%).
The American College of Radiology now recommends screening with mammography and MRI for women who’ve had cancer, who have dense breasts, or for women who were diagnosed with cancer before age 50, with all breast densities.
These recommendations are not routine in Canada, but experts recommend you advocate for yourself.
Check out DBC's Advocacy Tool Kit to help you advocate for the screening you need.
The information below shows some of the latest evidence on the benefits of additional screening. Feel free to copy, paste and print for your doctor.
Women with Dense Breasts Deserve the Right to Effective Screening
- Background
Canadian provinces and territories inform women of their breast density category. However, notification alone is not enough—women with dense breasts need supplemental screening, such as ultrasound, CEM, or MRI, for early cancer detection. Both category C and D women face increased risk and require additional screening to ensure early diagnosis and better outcomes.
- Risks of dense breasts
Dense breasts are normal and common but carry two significant risks:
- Increased cancer risk: Women with the densest breasts (category D) are four to six times more likely to develop breast cancer than those with fatty breasts (category A).
- Masking: Dense breasts make it harder for radiologists to spot cancer because both cancer and dense tissue appear white on a mammogram. The denser the breast, the greater the possibility that cancer will be missed on a mammogram. In fact, mammography misses 40% of cancers in women with category D density and 30% in category C.
Cancers missed on mammograms continue to grow and are often discovered only when a lump is felt. These are known as interval cancers, diagnosed between scheduled screenings. Interval cancer rates are 13 to 18 times higher in women with dense breasts and these cancers tend to be larger and more likely to have spread to lymph nodes. Consequently, these women often need more aggressive treatments and have poorer outcomes compared to those with screen-detected cancers. The purpose of screening is to detect cancers early to reduce deaths and suffering. Therefore, reducing interval cancers is a critical goal.
Individuals with non-dense breasts who undergo mammograms are 41% less likely to die from breast cancer compared to those who do not. In contrast, women with dense breasts who have mammograms are only 13% less likely to die. This disparity represents a life-threatening inequity, as individuals with dense breasts in Nova Scotia are underserved if mammograms are their only screening option.
- Evidence on supplemental screening: MRI, CEM, and Ultrasound
To reduce interval cancers effectively, supplemental tests like ultrasound or MRI should be offered. These modalities are proven to detect cancers missed by mammography when they are small and have not yet spread, and before they become interval cancers.
i). MRI Screening Supporting Studies:
- MRI has been proven to detect invasive cancers and reduce both interval cancers and late-stage disease in many studies.
- The DENSE trial in the Netherlands, an ongoing RCT, published results showing the interval cancer rate dropped to 0.8/1000 when MRI was added to mammography, compared to 4.9/1000 with mammography alone.
- A study from Memorial Sloan Kettering involving 2780 women at elevated risk screened with MRI and mammography showed no interval cancers, compared to 9 interval cancers among 4811 women screened with mammography alone.
- A Canadian study demonstrated a reduction in late-stage disease due to MRI screening in women with known pathogenic variants.
- MRI screening has increased the detection of biologically significant cancers.
Surrogate for Mortality Reduction: Reduction of interval cancers is considered an acceptable surrogate for breast cancer mortality reduction, which typically takes over 10 years to demonstrate in an RCT. In Europe, MRI is recommended for all women aged 50-70 with category D density. MRI is effective in finding more cancers than ultrasound. However, the focus on mortality alone overlooks the broader benefits of early detection. Early detection of breast cancer means a better prognosis, less aggressive treatment, better quality of life, and less cost to the healthcare system.
ii). Ultrasound Screening Supporting Studies:
- Research over the past three decades, including single-institution and multi-centre trials, has shown that supplemental ultrasound screening benefits women with dense breasts by improving the detection of node-negative invasive cancers and reducing interval cancer rates.
- Studies have shown that ultrasound detects an additional 2-3 cancers per 1000 examinations over mammography alone.
- The J-Start trial in Japan, an RCT that began in 2007, has shown that adding ultrasound to mammography finds more cancers, which are smaller and have not yet spread to the lymph nodes. The trial indicated that adding ultrasound reduced interval cancers by a factor of 4, with an interval cancer rate of 0.5/1000 in the group having mammography plus ultrasound compared to 2.0/1000 in the control group.
- Predictive Metrics: The decreased interval cancer rate in the study suggests a predicted reduction in mortality.
- It is unethical to allow women to die while waiting for RCTs in Japan and the Netherlands to mature, especially given the significant findings to date.
iii). Braid study-uk: A randomized control trial in UK recently published included 9000 women with dense breasts and negative 2D mammogram. They were randomized to 1 of 4 screening groups for supplemental screening; abbreviated MRI (Ab-MRI), automated whole breast ultrasound (ABUS), contrast-enhanced mammography (CEM), or no supplemental screening. All modalities significantly increased cancer detection. All cancers detected were small. Cancer detection rates for Ab-MRI, ABUS, and CEM were 17.4/1000, 4.2/1000, and 19.2/1000, respectively and recall rates were 9.7%, 4.0%, and 9.7%, respectively .
iv). Ontario Health report: In December 2023, Ontario Health released a comprehensive 293-page “Health Technology Assessment” on supplemental breast cancer screening. This assessment recommended supplemental screening due to its effectiveness in detecting more cases of breast cancer and reducing interval cancers in women with dense breasts (categories C and D). However, due to cost considerations, Ontario Health recommended publicly funding supplemental screening only for category D. At the time of the study, the cost analysis (Table 1) had not yet been published.
Currently, women with category D breast density in Ontario can request a requisition from their provider for an MRI every two years or an ultrasound every year, in addition to their mammogram, while the Ontario screening program works to make supplemental screening standard for category D.
v). Two studies from British Columbia: Research from British Columbia reveals seven additional cancers per thousand screenings that were not detected by mammography. Mammography typically finds five cancers per thousand. The additional seven cancers, missed by mammograms, would likely have progressed to interval cancers.
Another important Canadian study, recently published, shows that using ultrasound for women with dense breasts for both screening and surveillance after cancer, finds six cancers per thousand screens. This is more than double the rate in most other published studies, primarily from the USA. This is, partly because in the US, women have annual mammograms, whereas in Canada, most women only have biennial mammograms, and because in the US, screening mammography is increasingly done with 3-D technology. So, there are more cancers, not found on mammography in Canada than in the US.
- Cost savings in treatment from early detection
MRI as a supplemental screening tool effectively reduces interval cancers, making it cost effective. That is part of the rationale used by EUSOBI and Ontario Health to recommend breast MRI for women with category D breasts. The cost of treating advanced cancer has increased exponentially in the last several years, driven by the high cost of new, beneficial drugs. Recently published Canadian research shows that there are large reductions in treatment costs when cancers are detected earlier. Table 1 shows the cost of treatment by stage and subtype. The mean treatment cost for a Stage 1 patient is $39,000, compared to $371,000 for a Stage 4 patient. For women with Her2-positive Stage 4 cancer, treatment costs can exceed $500,000.
- Jurisdictions
Canada: Residents of British Columbia, Alberta, Saskatchewan, NWT, or Ontario, can access supplemental screening to varying degrees. Outside of Canada: Many US states are offering supplemental screening. As well, as shown in the chart compiled by DenseBreast-info.org, several countries have made supplemental screening a standard practice.
- Recommendations
The benefits of supplemental ultrasound, CEM, or MRI for early detection in individuals with dense breasts are evidence based. These screenings significantly reduce interval cancer rates, as confirmed by robust research.
Given the clear evidence supporting additional screening for those with dense breasts, it's time for all provinces/territories to align with leading practices and ensure equitable access to early detection methods for all. Not only would this promote health equity but also reduce healthcare costs and the burden of late-stage cancer treatment.

Screening for Canadian Women with Dense Breasts
Les tests de dépistage suivants sont décrits ci-dessous : mammographie, échographie, échographie 3D (ABUS), IRM, tomosynthèse.
La mammographie réduit la mortalité du cancer du sein, mais c’est un outil de dépistage imparfait pour les femmes aux seins denses car elle peut manquer des tumeurs cancéreuses dans les seins denses.
Dans 40 % des cas, les mammographies peuvent ne pas détecter le cancer dans les seins les plus denses. Par conséquent, les femmes avec des seins denses devraient envisager des tests de dépistage supplémentaires en complément à leur mammographie. Une échographie ou une IRM en complément à une mammographie augmente considérablement le taux de diagnostic du cancer chez les femmes avec des seins denses.
Au Canada, il n’est pas facile d’avoir accès à des tests de dépistage supplémentaires. Vous devrez peut-être défendre vos droits.
Qu’est-ce que c’est? La mammographie permet de radiographier des seins sur plusieurs angles. C’est le seul moyen qui peut déterminer la densité mammaire.
Points positifs: Au cours des 30 dernières années, la mammographie a permis de réduire de 35 % le nombre de décès par détection précoce.
Limites: Chez les femmes avec des seins denses, les tissus denses et le cancer apparaissent en blanc sur une mammographie, ce qui rend difficile la détection du cancer. La mammographie utilise des rayonnements à faible dose.
Accessibilité: La mammographie de dépistage est disponible partout au Canada, sauf au Nunavut. La mammographie numérique est largement disponible et elle est plus précise que la mammographie analogique en ce qui concerne les seins denses.

Qu’est-ce que c’est? L’échographie utilise des ondes sonores à haute fréquence pour produire des images du sein.
Points positifs: Lorsqu'elle est utilisée avec la mammographie, l'échographie augmente le taux de détection du cancer jusqu'à 97 %. L’échographie détecte 2 à 3 cancers supplémentaires pour 1000 femmes. Elle peut détecter le cancer dans les seins denses à un stade précoce. C'est rapide, sûr et non invasif. Aucune radiothérapie n'est impliquée.
Limites: L’échographie est un test très sensible, généralement utilisé à des fins de diagnostic et non de dépistage. Elle peut détecter des anomalies qui nécessitent un examen approfondi. L’échographie seule n’est pas recommandée comme outil de dépistage du cancer du sein.
Accessibilité: Une ordonnance pour une échographie n’est généralement pas émise à moins qu’on constate un résultat suspect sur une mammographie, une IRM ou un examen clinique des seins. Il pourrait y avoir une clinique privée dans votre ville qui ne demande pas une ordonnance d’un médecin ou d’une infirmière praticienne. MISE À JOUR : En Colombie-Britannique, l’échographie de dépistage est maintenant couverte par le régime de services médicaux (Medical Services Plan) pour les femmes avec des seins denses si le médecin de famille ou l’infirmière praticienne leur fournissent une ordonnance.

Qu’est-ce que c’est? Il s’agit d’une échographie 3D. Des ondes sonores reconstituent les images du sein en 3 dimensions.
Points positifs: ABUS can find small, invasive, node-negative cancers missed by mammography. It is radiation free.
Limites: ABUS may identify abnormalities that are not seen on a mammogram. Some of these abnormalities may require additional ultrasound or biopsy. Remember most abnormalities are not cancerous.
Accessibilité: Currently, ABUS can be found for screening purposes in Ontario, Alberta, and British Columbia.
In Ontario, there is one location in Toronto that performs screening ultrasound with ABUS. The clinic performs breast imaging and more and is called Toronto Centre for Medical Imaging. Patients wanting ABUS must pay out of pocket but some private/group insurance plans may cover part of the cost. No requisition is needed, but it is recommended to bring a CD with your latest mammograms (unless you are on Pocket Health and can email it) We are not affiliated with the clinic, so please direct any questions to them.
In Alberta, ABUS is covered under the provincial health insurance plan (AHIC) for women with dense breasts. Many clinics offer ABUS.
In British Columbia, ABUS is covered under the provincial health insurance plan for women with dense breasts (Category C and D). It is available in Victoria at West Coast Imaging. A requisition is needed. Please contact the clinic if you want more information.


Qu’est-ce que c’est? Également connue sous le nom de mammographie 3D, la tomosynthèse réalise plusieurs fines coupes d’images de sorte que les tissus qui se chevauchent sont moins susceptibles de masquer une tumeur cancéreuse. La patiente est placée exactement dans la même position que pour une mammographie ordinaire.
Points positifs: Par rapport à la mammographie numérique, la tomosynthèse augmente le taux de détection des tumeurs invasives de 1 à 2 cancers supplémentaires pour chaque 1 000 femmes. Utilisée en complément à la mammographie, la tomosynthèse diminue le taux des faux positifs.
Limites: Dans les seins denses, la tomosynthèse ne détecte pas autant de cancers que l’échographie. La dose de radiation peut être plus élevée que celle d’une mammographie ordinaire, car l’acquisition d’images prend plus de temps. Lorsque la tomosynthèse est utilisée en complément à la mammographie, la dose de radiation est légèrement plus que le double de celle de la mammographie ordinaire.
Accessibilité: À l’heure actuelle, la tomosynthèse est surtout utilisée à des fins de diagnostic après la découverte d’une anomalie. Toutefois, en Alberta, les patientes de certaines cliniques font l’objet d’un dépistage au moyen d’une mammographie 2D et d’une tomosynthèse. Des études cliniques sont en cours au Canada visant à évaluer le rôle de la tomosynthèse dans le dépistage du cancer du sein.
Qu’est-ce que c’est? A standard iodinated contrast agent is used; the same contrast used for CT scans. Cancer cells take up the contrast agent, which absorbs X-rays, so the cancer appears white on the mammogram.
Points positifs: Is lower cost than MRI and can detect cancers that are not visible on a standard mammogram. The cancer detection rate is close to MRI.
Limites: Uses slightly more radiation than a standard mammogram. Women with poor kidney function or who have had a previous allergic reaction to contrast agents might be advised to avoid this test.
Accessibilité: Is available in many locations across Canada.
- The term you’ll hear now is that women should be “breast aware,” which means pay attention to how your breasts look and feel.
- You should be familiar with the shape of your breasts and know what your normal breast texture feels like.
- Puckering is sometimes more visible if you look in the mirror with your arms raised. You can check your breasts lying in bed or in the shower. Soapy hands make it easier to slide your hand along the skin and make it easier to notice normal
texture or a lump. - Some cancers are not detectable on mammograms, so breast self-exams are worth doing, especially if your mammograms are done less than once per year. By getting to know what your normal breast feels like, you’ll know if there’s a change. Check out www.knowyourlemons.com
SeinFormer, c’est vital ! Lisez nos guides et rapports
Dépistage : comment se comparent les provinces et territoires selon 7 pratiques essentielles ?
Obtenir les faits. Pourquoi les directives de dépistage du cancer du sein sont trompeuses et dangereuses?
The 2018 breast cancer screening guidelines were made by a panel of 14 members selected by the Public Health Agency of Canada and the College of Family Physicians of Canada.
Le groupe ne comprenait aucun expert en dépistage du cancer du sein. Le groupe comprenait un psychologue, un ergothérapeute et un néphrologue (spécialiste des reins), des médecins de famille, des infirmières, un chiropraticien et un médecin d’urgence. Les lignes directrices ont ignoré la contribution d’experts en diagnostic et traitement du cancer du sein. did not include any experts in breast cancer screening. The panel included a psychologist, an occupational therapist and a nephrologist (kidney specialist), family doctors, nurses, a chiropractor, and an emergency room doctor. The guidelines ignored the input of experts in breast cancer diagnosis and treatment.
Le groupe d’étude a déclaré que la présence d’un expert en diagnostic du cancer du sein risquerait de fausser l’élaboration des lignes directrices. Le groupe d’étude a laissé entendre que puisque les experts gagnent leur vie par le diagnostic de cancers du sein, ils vont passer leur profit financier avant le bien-être des patients. Nous sommes fortement en désaccord. Au Canada, nos radiologistes ont des listes d’attente et leurs salaires ne sont aucunement liés à plus grande demande.
The guidelines are used by Canadian family doctors and nurse practitioners. The guidelines pertain to screening for 9 million women, aged 40-74. Many provincial health agencies have adopted the guidelines in their policies. The guideline is being reviewed in 2023.
Des milliers d’experts sont de l’opinion que les lignes directrices devraient être rejetées. Les 2 000 membres de l’Association canadienne des radiologistes ont publié une déclaration rejecting the guidelines. CAR is expected to publish its own guidelines shortly.
La Société canadienne de l’imagerie mammaire a publié une déclaration rejetant les lignes directrices.
Here are just a couple of the Op-Eds written by breast cancer screening experts:
The guidelines are not based on current science. The studies used to make the guidelines are 30-50 years old and the technology used is obsolete. One of the major studies used was flawed and had compromised randomization (CNBSS). The guidelines underestimate the benefits of mammography, overstate the harms and ignore the risks of dense breasts.
Voici pourquoi les femmes dans leur quarantaine ont besoin de mammographies :
- L’incidence du cancer du sein augmente à l’âge de 40 ans
- 16 % des cancers du sein surviennent chez les femmes dans leur quarantaine
- La moitié des cancers mortels sont diagnostiqués avant l’âge de 49 ans
- Women who screen in the 40s are 44% less likely to die from breast cancer than women who do not have mammograms
The evidence supports women in their 40s being screened.
Selon 2 modèles, le Dr Martin Yafa et la Dre Nicole Mittman ont estimé que 400 femmes perdront leur vie chaque année au Canada si la recommandation du non-dépistage par le Groupe d’étude est suivie.
Une étude canadienne portant sur 2,8 millions de femmes faisant l’objet d’un dépistage du cancer du sein depuis plus de 20 ans a montré que les femmes de 50 à 70 ans avaient un taux de décès 40 % plus bas que les femmes n’ayant pas subi de mammographie. Cette étude démontre aussi que les femmes âgées de 40 à 49 ans affichaient une baisse de 44 % du taux de mortalité par cancer du sein avec leur participation au dépistage [mammographie].
Une étude récente réalisée en Suède a montré une baisse de 60 % du taux de mortalité au cours des 20 premières années après un diagnostic de cancer, et une baisse de 47 % du taux de mortalité au cours des 20 années suivant un diagnostic de cancer, chez les femmes qui ont subi une mammographie, comparé aux femmes qui n’ont subi aucune mammographie.
Quels sont les désavantages aux femmes dont le Groupe d’étude le leur demande de considérer
A) L’angoisse causée par un résultat faux-positif ?
Le terme « faux-positif » est un mésusage par le Groupe d’étude. On pourrait penser que cela signifie qu’une femme a été informée qu’elle a un cancer, alors que ce n’est pas le cas. Le Groupe d’étude utilise ce terme lorsque le résultat de la mammographie détecte quelque chose, et la femme doit retourner pour d’autres examens pour déterminer si elle a le cancer ou non. La grande majorité de ces femmes n’ont pas le cancer. Selon le résultat de l’imagerie supplémentaire, une biopsie à l’aiguille avec anesthésie locale est parfois réalisée. Un degré minimal de malaise sera ressenti.
Sans aucun doute, le rappel induit un certain stress, mais ce stress s’est avéré de courte durée et est résolu lorsque les résultats négatifs de l’imagerie sont obtenus. Habituellement, lorsqu’elles sont informées de la situation, la plupart des femmes sont prêtes à faire face au stress plutôt que de courir le risque de manquer le diagnostic d’un cancer qui pourrait raccourcir leur vie ou qui lui ferait subir un traitement plus agressif.
B) Surdiagnostic
Le surdiagnostic est la possibilité théorique que certains cancers découverts par le dépistage restent inoffensivement cachés dans le corps jusqu’à ce que la femme meure d’une autre cause. Il est probable que cela se produit dans une certaine mesure, mais cela ne peut qu’être estimé. Le Groupe d’étude exagère l’incidence du surdiagnostic. La plupart des experts estiment qu’il se situe entre 1 % et 10 %. Un surdiagnostic est plus plausible chez les femmes âgées, qui peuvent avoir d’autres maladies (maladie du cœur) et même d’autres cancers, qui pourraient être la cause de leur mort avant le cancer du sein. Mais la probabilité de surdiagnostic est infiniment petite chez les plus jeunes femmes.
The decision whether to participate in screening is up to individual women with advice from their health care provider. For there to be true shared decision-making, both a woman and her physician need to have clear and accurate information on the benefits and harms of screening. Read below the misinformation Canadian experts are trying to dispel amongst women and physicians.
Addressing Misinformation about the Canadian Breast Screening Guidelines
You’re in your 40s and you’ve decided you’d like a mammogram, but in your province women in their 40s need a requisition. Your health care provider will not give you one or needs to be convinced. Or you’re in your 40s and you’ve decided you’d like a mammogram. You can self-refer in your province, but your health care provider dismisses the importance of you having a mammogram. We’ve designed a script to help you advocate for yourself and overcome any potential barriers while having a conversation with your health care provider. PLEASE NOTE IN JULY 2023, The Task Force published a newsletter where it stated that following a conversation between patient and provider, if a woman chooses to have a mammogram, she should have a mammogram. This is the clearest messaging to date from the Task Force that the decision to screen is a woman's and she should not be denied a requisition if she wants one.
If your health care provider says: The Canadian breast cancer screening guidelines do not recommend mammograms for women in their 40s.
You can respond: I understand that is the recommendation but it also states, that the decision whether or not to have a mammogram is a woman’s and that depends on the values she places on any possible benefits and harms.[1] Therefore, based on my values, this is my decision and I’ve decided to get a mammogram.
If you need a further response: You can use this quote from Task Force vice-chair Dr. Ainsley Moore, “The new guidelines are intended for an empowered position, which puts the decision-making in the hands of the individual woman in terms of what she prioritizes.”[2] Based on a woman’s values and preferences, the decision to undergo screening is conditional on the relative value a woman places on possible benefits and harms from screening. Please also refer to the July 2023 Task Force newsletter where it conveys the final decision is a woman's.
If your health care provider says: You don’t have a family history or other risk factors and so you don’t need to start screening in your 40s.
You can respond: I’m aware that the biggest risk factor for breast cancer is being a woman and that over 75% of women diagnosed with breast cancer have no risk factors.
**If it applies to you, you can remind your health care provider that Black, Asian and Hispanic women are at an increased risk for breast cancer at a younger age than white women.[3]
If your health care provider says: Having a mammogram can result in a “false positive”, meaning you may be recalled for more testing. These tests can create anxiety for you.
You can respond: I understand there’s a chance that more tests will be needed after my mammogram to make sure there is no cancer, but I’m not very worried about being recalled. I understand that less than 10% of women are recalled.[4] I’d rather be safe than sorry. I understand any anxiety I experience will be short-lived if I have a normal result. And if the result is not normal, I’d prefer to have cancer found at an early stage, rather than a later stage.
If your health care provider says: Having a mammogram can result in over-diagnosis. That means finding a cancer that if left untreated would never cause you any harm, but if detected requires treatment and surgery.
You can respond: I understand and I’m willing to accept that I may be treated for something that might never have become a problem if left untreated. Again, better safe than sorry.
If your health care provider says: This graphic shows that out of 1000 women who have a mammogram, only 1 life is saved.
Your response: I learned the Canadian Society of Breast Imaging states 2 lives are saved.[5] I also know that finding cancer early means I may avoid harsh medical treatments like chemotherapy and mastectomy that can reduce the quality of my life.
As stated in the Canadian guideline, the decision to have a mammogram is yours and therefore you have a right to have a mammogram in your 40s, no matter what province you live in.
[1] https://canadiantaskforce.ca/guidelines/published-guidelines/breast-cancer-update/
[2] https://www.ctvnews.ca/health/mammogram-guidelines-now-consider-women-s-personal-values-not-just-age-risk-1.4211240
[3] https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5875337/?tool=pmcentrez&report=abstract
[4] http://www.bccancer.bc.ca/screening/breast/results
[5]https://csbi.ca/education/